Here’s something that would be cool: a wearable continuous monitor for hormone levels. You could answer so many questions!
How do estrogen and progesterone change throughout the menstrual cycle? How do they correlate to mood, sexuality, premenstrual symptoms, etc? How do reproductive hormone levels change in response to hormonal birth control?
How do female reproductive hormones change during menopause? How do hormone levels correspond to menopause symptoms?
What exactly is going on with sex hormone levels, hour by hour, in trans people taking various hormone regimens? How do hormone levels correspond with various body changes?
How do insulin levels respond to diet, exercise, sleep, or other lifestyle factors?
How do cortisol levels correlate to subjective stress? How much do different stressful or relaxing situations affect cortisol levels?
To answer any of these questions easily, we need a non-invasive way to measure circulating hormone levels. It’s inconvenient to take frequent blood tests. And when hormones fluctuate on a daily and/or monthly cycle, as many do, taking single snapshots can’t measure change very accurately.
So, why don’t we have wearable hormone sensors already?
The most common way to measure hormone levels in bodily fluids is an immunoassay. An antibody is found that binds to the hormone in question; these antibodies are linked to some marker that will luminesce, or change color, when the hormone is bound. The intensity of the color or luminescence is then a measure of the hormone concentration.
One familiar example of an immunoassay is a pregnancy test. The test line turns purple in the presence of the pregnancy-associated hormone hCG in the urine sample.
While immunoassays are ubiquitous, cheap, portable, and produce quick results, they’re not generally reusable. A pregnancy test is single-use; once the line has turned purple, it doesn’t fade back to white. This makes it poorly suited for continuous monitoring.
Impedance Spectroscopy
An alternative method for detecting the concentrations of biomolecules is impedance spectroscopy.
The impedance curves in response to an oscillating electric field differ between different materials, including different concentrations of various biomolecules in aqueous solution.
Impedance spectroscopy has been shown to be effective at measuring concentrations of progesterone1, estrogen2, cortisol3 , and insulin4 in solution.
These methods depend on coating an electrode with antibodies to the desired hormone. Impedance measurements will then have a dose-response relationship with the amount of hormone that binds to the antibodies on the electrode.
Impedance Spectroscopy in Sweat
Impedance spectroscopy can be applied to sensing the presence of biomarkers in sweat. Sweat has the advantage that it can be collected noninvasively, unlike blood.
Steroid hormones, such as cortisol, estrogen, and testosterone, show strong correlations between serum concentration and sweat concentration, making sweat measurements a good proxy for blood measurements.5
An impedance-spectroscopy sensor for cortisol, containing a gold electrode coated with cortisol antibody, was able to distinguish between concentrations of cortisol in the nanograms/mL range in human sweat. It could also report measurements continuously at a rate of one measurement per minute.6
An impedance spectroscopy sensor for IFN-gamma (a protein marker of inflammation) in sweat, using antibodies for IFN-gamma bound to an electrode, was able to distinguish concentrations at the picogram/mL level. In a human study of 8 healthy individuals, there was a correlation of 0.98 between the standard Luminex immunoassay measurements of sweat IFN-gamma and the sensor’s measurements.7
A wearable impedance spectroscopy sensor for the inflammatory markers IL-1-beta and CRP was able to achieve correlations of 0.99 and 0.95, respectively, with traditional immunoassay measurements. In a study on 20 subjects who wore a sweat-sensing device for a week, it was able to measure concentrations at a rate of at least 1 measurement per minute, and maintained stable levels over time, as expected.8
Who’s Working On It?
EnLiSense is a startup producing a wearable sweat sensing device, based on the research of Shalini Prasad, bioengineering professor at the University of Texas at Dallas. They participated in a biotech incubator competition in 2019 and received “over $1M” in federal funding, but don’t appear to have received other investment.
Apart from that, there don’t seem to be any other companies producing wearable hormone monitors.
Wei Gao, assistant professor of medical engineering at Caltech, and Alberto Salleo, professor of materials science at Stanford, have both published prototype wearable cortisol sensors, but have not as yet commercialized them to my knowledge.
What’s Left To Do?
The hardest technical problem — demonstrating that accurate, consistent measurements of hormone levels can be made in near-real-time from human sweat — seems to be mostly solved.
Getting the sweat, once a major challenge, seems to be possible today. Flexible skin patches with microfluidic channels can collect small quantities of sweat and guide it to flow over electrode sensors via capillary action.
And detection also seems to be feasible. Electrochemical sensing via wearable electrodes can rapidly detect analytes in the small volumes and small concentrations found in human sweat.
But prototype “wearable sensors” in the academic literature are not always completely self-contained — they need some separate lab equipment to actually measure analyte concentrations.
Also, of course, there’s development work involved in taking any hardware device from prototype to mass production and consumer usability.
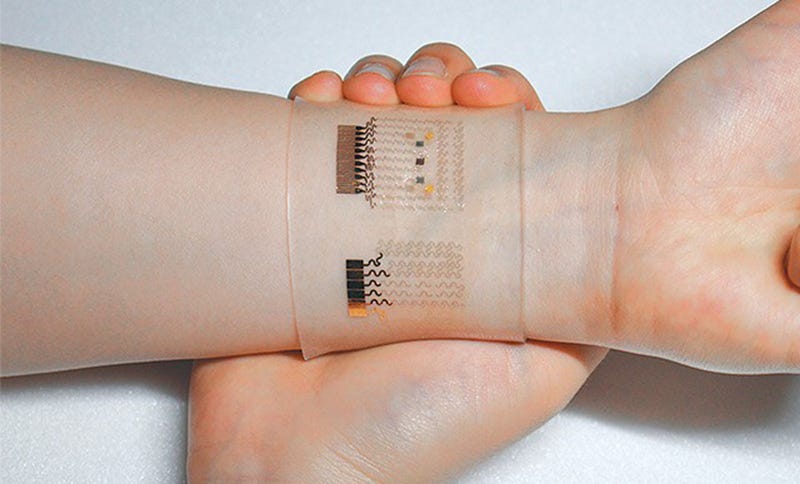
Gao’s wearable cortisol sensor: not a consumer-ready device yet!
But ultimately, it doesn’t seem that there are big unsolved technical problems left at this point.
And the consumer market for a FitBit-like hormone-sensing device might be quite substantial:
Women concerned about hormonal birth control side effects
Women dealing with menstrual-related symptoms
Menopausal women
Infertile couples
Men on testosterone replacement treatment
Trans people
Fitness-conscious gadget lovers
It’s also possible to go down the FDA approval route as a medical device, which appears to be what EnLiSense is doing, with applications such as COVID-19 detection and IBD flare-up detection.910
But I hope someone tries to go down the direct-to-consumer route as well; it’s probably quicker, and the reproductive-hormone-tracking use cases are really valuable to healthy people.
Zia, Asif I., et al. "Sensor and instrumentation for progesterone detection." 2012 IEEE International Instrumentation and Measurement Technology Conference Proceedings. IEEE, 2012.
Im, Ji-Eun, et al. "Electrochemical detection of estrogen hormone by immobilized estrogen receptor on Au electrode." Surface and Coatings Technology 205 (2010): S275-S278.
Ganguly, Antra, et al. "Autonomous, real-time monitoring electrochemical aptasensor for circadian tracking of cortisol hormone in sub-microliter volumes of passively eluted human sweat." ACS sensors 6.1 (2020): 63-72.
Malkoc, Aldin, et al. "Enhancing glycemic control via detection of insulin using electrochemical impedance spectroscopy." Journal of diabetes science and technology 11.5 (2017): 930-935.
Chung, Michael, Giuseppino Fortunato, and Norbert Radacsi. "Wearable flexible sweat sensors for healthcare monitoring: a review." Journal of the Royal Society Interface 16.159 (2019): 20190217.
Sankhala, Devangsingh, Sriram Muthukumar, and Shalini Prasad. "A four-channel electrical impedance spectroscopy module for cortisol biosensing in sweat-based wearable applications." SLAS TECHNOLOGY: Translating Life Sciences Innovation 23.6 (2018): 529-539.
Kothari, Aashay, et al. "An observational study for detection and quantification of interferon-γ in sweat toward inflammation monitoring." Biosensors and Bioelectronics: X 10 (2022): 100122
Jagannath, Badrinath, et al. "A sweat-based wearable enabling technology for real-time monitoring of IL-1β and CRP as potential markers for inflammatory bowel disease." Inflammatory Bowel Diseases 26.10 (2020): 1533-1542.
https://dallasexpress.com/wearable-device-monitors-infection-covid-19-exposure/
https://www.gastroendonews.com/In-the-News/Article/05-21/IBD-sweat-sensor/63431





I don't want to tamp down the enthusiasm too much, but I'm not sure the technical hurdles here have actually been solved. I'd like to see input from an actual biochemist, but I have some experience with hormone therapy and had to learn a fair amount about why we get the specific blood tests we do, when they are and aren't reliable, etc. Human sex hormone concentrations are very low. A normal cortisol level is about 20 mcg/ml, where a normal estradiol range for a woman is 25-350 pg/dl. That's a five orders of magnitude difference. This is why you typically need multiple draws to qualify for therapy and it impacts how much blood they need to draw. When concentrations get low enough, they need to ensure they drew enough to detect anything at all. Being able to detect what normally takes a full vial out of a drop of sweat seems questionable.
On the other hand, pregnancy, sure maybe, because estradiol absolutely shoots through the roof when you're pregnant. In the area of a thousand times the normal concentration.
It would be pretty amazing to be able to tell if you were pregnant on the same day the egg implants...